Many people don’t realize that lung cancer is the leading cause of cancer deaths in the U.S. In fact, it’s responsible for more deaths than colon, breast, and prostate cancers combined. Three out of four people are diagnosed with lung cancer at an advanced stage when it’s harder to treat, according to a 2026 report by the American Cancer Society.
Another concerning trend is that lung cancer cases have been increasing among younger adults, particularly women and people of Asian descent, as well as those who have never smoked.
[time-brightcove not-tgx=”true”]
So why isn’t there routine screening for lung cancer like there is for many other forms of cancer? Here’s what experts say.
Who currently gets screened?
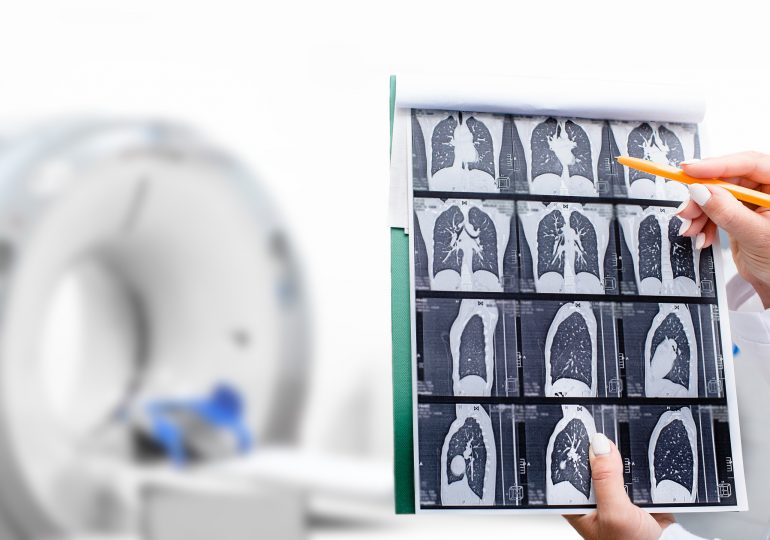
The U.S. Preventive Services Task Force (USPSTF), an independent panel of national experts in evidence-based medicine, recommends annual screening for lung cancer with a low-dose CT (computed tomography) scan in only select populations. This includes adults ages 50 to 80 years who have a 20 pack-year smoking history and who either currently smoke or have quit within the past 15 years. (A pack-year equals smoking one pack—or about 20 cigarettes—per day for a year.).
But some experts believe these guidelines should be broadened.
“The current guidelines for lung cancer screening are based on a very outdated model for risk assessment,” says Dr. Ankit Bharat, chief of thoracic surgery and executive director of the Canning Thoracic Institute at Northwestern Medicine. “It presumes smoking is the only cause of lung cancer. Anyone exposed to secondhand smoking, air pollution, or radon—risk factors that are well established—doesn’t have any way of getting screened.”
Read More: Why Are People Obsessed With Hypochlorous Acid?
In a study published in a November 2025 issue of JAMA Network Open, Bharat and his colleagues examined the records of nearly 1,000 people treated for lung cancer and discovered that only 35% of them met the USPSTF criteria for screening. If lung cancer screening were expanded to include all people ages 40 to 85, the researchers estimate that this would detect 94% of lung cancers, preventing at least 26,000 deaths annually.
“People have to understand that if they don’t smoke, they’re not immune to lung cancer,” Bharat says. “Early detection is the only way to treat early-stage lung cancer. Stage I lung cancer is completely curable, and treatment is an outpatient procedure.”
There’s no question that “screening definitely saves lives, and finding it early makes a difference,” says Dr. Roy Herbst, chief of medical oncology and hematology at the Yale Cancer Center.
Obstacles to lung cancer screening
Even within the current guidelines, most people who are eligible to get screened don’t get checked out. “The primary reason is lack of public awareness,” says Dr. Samir Makani, medical director of the lung cancer screening program at the Scripps Cancer Center and an interventional pulmonologist at Scripps Memorial Hospital Encinitas. “Research shows that less than 20% of eligible people are getting screened. Responsibility for achieving greater awareness of lung cancer and the impact of lung cancer screening falls on all of us—patients, primary-care physicians, and the U.S. health-care system as a whole.”
Part of the problem may be that getting screened is a “cumbersome process,” as Makani puts it. “With lung cancer screening, you need to undergo a shared decision-making visit [with your doctor] to discuss the risks and benefits, then go get a CT scan.” In other words, it’s a two-step process, compared to simply getting an order for a mammogram or colonoscopy, for instance.
One of the arguments against expanding screening is that it will simply cost too much. Yet Bharat points out that “the cost of treating someone with Stage I lung cancer is a fraction of the cost of treating Stage IV lung cancer.”
Read More: Do Compression Socks Actually Work?
People are also concerned about being exposed to radiation with low-dose CT scans. “We don’t want to give people radiation exposure unnecessarily,” says Herbst. But the amount of radiation exposure is quite low—only slightly higher than with a mammogram.
There are also concerns about incidental findings on these CT scans. “We can find things that are not lung cancer—it could be a benign lesion or a fungal infection that causes a nodule that’s harmless,” says Dr. Kim L. Sandler, a professor of radiology at Vanderbilt University Medical Center and director of the Vanderbilt Lung Screening Program. The possibility of incidental findings may concern some patients, but “incidental findings can be beneficial if they’re actionable,” she notes.
Besides, there’s another potential upside to low-dose CT screening for lung cancer: A single scan can assess heart and bone health, too, by providing cross-sectional images of the whole chest cavity, including the heart and thoracic spine .
A push for universal lung cancer screening
Bharat thinks lung cancer screening should be universal after age 40, regardless of whether people have a history of smoking. Many other experts agree.
Sandler notes that with a universal approach, the interval for subsequent low-dose CT screenings would differ based on people’s personalized risk. “We have personalized recommendations for colon and breast cancer [screening] based on people’s risk factors,” says Sandler. “We need to find out how to do that with lung cancer as well.”
Until the screening recommendations are broadened, it’s important for people to be proactive about this issue, experts agree. “If you’re eligible to get screened, get screened,” Herbst says. “If you have a family history of lung cancer, discuss it with your doctor.”
Read More: The 1-Minute Trick to Calming Down Your Nervous System
Also, if you’ve ever smoked or had a prior cancer, particularly breast cancer, be sure to discuss it with your doctor, Sandler says. And be sure to bring persistent symptoms such as a chronic cough to your doctor’s attention.
While insurance coverage for low-dose CT lung cancer screening tracks closely with the USPSTF recommendations, your doctor may be able to get you coverage even if you don’t fit the parameters. A physician can make a clinical decision based on their concerns about your risk for lung cancer and could prescribe a CT scan or help you find an affordable option near you if you’ll be paying out of pocket, Makani says. The out-of-pocket cost is often $300 to $500, he says.
“The most important part of lung cancer screening is the survival benefit,” says Makani. The five-year survival rate for Stage IA lung cancer is upwards of 90%, he says, compared to 20% for Stage III. This is especially important, he adds, because “the majority of patients we find lung cancer in are asymptomatic.”
Leave a comment